Book an Appointment
(02) 93 000 999
Gum diseases are infections of the gum that range from mild inflammations of the gums (gingivitis) to major damage of the bone and tissues supporting your teeth (periodontitis).
Whilst regular brushing and flossing will prevent bacteria and plaque build-up on your teeth, plaque on your teeth and gum line that is not removed can infect the gums and lead to symptoms of gingivitis, the first stage of gum disease.
When gingivitis occurs, your gums may become red, swollen and bleed while brushing. The good news is that gingivitis is the early stage of the disease and usually responds well to good brushing and flossing habits and regular visits to your dentist for cleaning.
If you experience bleeding, pain or swelling in your gums – don’t delay seeing your dentist, as a minor case of gingivitis can lead to a major case of periodontitis. In the worst scenario, you may even lose your teeth.
Visit our online booking page or contact us on (02) 9300 999 to help us prevent or manage your gum disease symptoms.
Remember, the best way to prevent gingivitis us to maintain proper brushing and flossing habits and visiting your dentist every 6 months for cleanings and a checkup!
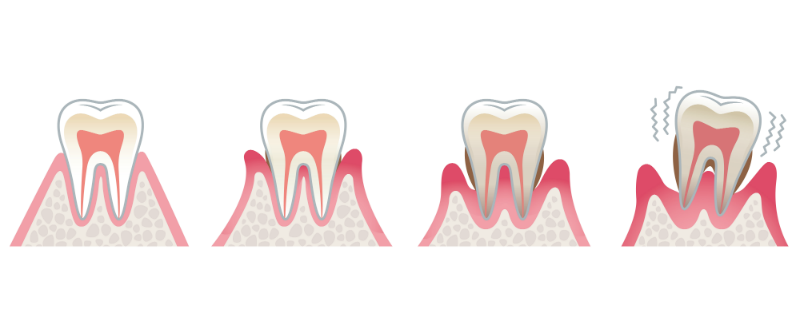
Gingivitis occurs when bacteria causes your gums to become red, swollen and bleed while brushing. Inflammarion is your body’s natural response to these bacteria and their toxins. The good news is that gingivitis is a milder form of gum disease that can usually be treated by observing daily dental hygiene and by regular cleaning by your dentist. Simple gingivitis does not usually result in any loss of bone and tissue that hold your teeth in place.
If gingivitis is left untreated, the plaque build-up hardens and causes your gum to detach from the tooth. This forms a ‘pocket’ between the tooth and gum, encouraging further plaque build-up in these infected pockets. The hardened plaque slowly destroys your bone and periodontal ligaments, which are responsible for supporting your teeth. Your teeth may eventually become loose and have to be removed.
Healthy gums are pink in colour with no redness, inflammation or tenderness. They do not bleed while brushing.
If you experience some or all of the following symptoms, you may have gingivitis:
bleeding gums
bad breath
inflammation – red, swollen or tender gums that bleed during brushing
visible plaque on the teeth that can be removed by brushing or dental cleaning.
Periodontitis includes the symptoms of gingivitis and also some, or all, of the following symptoms:
loose teeth;
a ‘pocket’ formed between the root and gums of over 4mm. Healthy teeth usually have pocket depths of between 1mm and 3 mm;
Receding gums or the appearance that your teeth are getting longer.

The most suitable treatment option for you will depend on the extent of your gum disease and how long you’ve waited before seeking treatment. At Dentist Mandy, we will sit down and conduct a thorough examination of your teeth and gums before providing the most appropriate treatment for your condition.

If your gum disease is mild or moderate, a non-surgical, deep-cleaning technique called root planning may be sufficient. The dentist will numb the gum under local anaesthetic before scraping off the plaque and tarter above and below the gum line. The dentist will typically work on a quarter of your mouth at a time, so you may need 2 to 4 appointments to complete the treatment.
The success of the treatment will depend on factors such as:
The severity of the disease
Extent of bone and tissue loss
Your brushing and flossing habits
Smoking habits
If your gum disease is severe, surgical treatment may be required and we may refer you to a specialist for treatment.
After the root planing procedure, the ‘pocket’ between your gums and teeth will shrink and heal. However, one side effect you may experience is gum recession, resulting in your teeth becoming more sensitive to hot and cold temperatures.
You may experience mild to moderate discomfort for a few days after the treatment which can be managed by antibiotics, pain medications, anti-bacterial rinses and anti-inflammatories.
Contact your dentist if you experience any unusual symptoms post-treatment such as excessive bleeding, pain, swelling or bruising.
No. Healthy gums will not bleed when you brush and floss normally. If your gums are bleeding when you brush and floss, it may indicate gum disease. Regular visits to the dentist is recommended. Once treatment proceeds to remove the active disease and stabilise the inflammation of the gums, a professional lesson on how to brush and floss your teeth will maintain good oral hygiene habits and a healthy smile!
A healthy mouth should have gums fit snugly around each tooth. The distance between the gum tissue and its attachment to the tooth should be only 1 to 3 millimetres in depth. However, when gum disease occurs, it can lead to deeper spaces around your teeth. These are pockets, or more specifically, periodontal pockets. If gum disease is left untreated, the pockets will gradually deepen and potentially lead to tooth loss.
Food particles and bacteria in your mouth stick onto your teeth to form a sticky film layer called plaque, especially around the gum area. When plaque is not brushed away or flossed out, it will eventually harden into tartar. Tartar can only be removed by a dental professional. However, when left untreated, toxins will start to form on the tartar, causing inflammation and swelling. This will then result in a pocket formation between the teeth and gums. When more and more tartar builds up, it will further deepen the periodontal pockets.
